Divarication of Rectus Abdominis muscles (also known as “rectus diastasis” or DRAM)
Although pregnancy is an exciting time for most, it can be a confusing time for others. As women go through numerous physical changes there is an abundance of information available as to the different conditions some may experience.
It can be difficult sifting through the information and knowing what is reliable and what is not. A topic that receives a lot of attention online is abdominal separation during pregnancy.
During the antenatal period many women experience abdominal separation, also known as diastasis rectus abdominis, DRA or DRAM. DRAM is most commonly related to pregnancy although it can occur in other populations. During the 2nd trimester of pregnancy 33% of women exhibit this condition, increasing to 100% of women by the 3rd trimester.
What is DRAM?
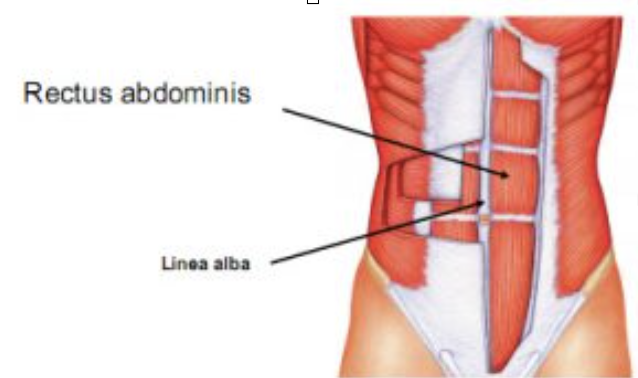
The rectus abdominis muscle is comprised of two rectus bellies. DRAM is the widening of these muscles at the linea alba (connective tissue that holds these muscles together). Throughout pregnancy the uterus expands to accommodate for the growing fetus. Due to hormonal changes and increases in spatial demand, the linea alba softens and the distance between the two muscle bellies increase. This increase in distance of the two bellies of the rectus abdominis is known as DRAM. This condition is a normal part of pregnancy and will generally recover within the first 8 weeks post delivery with natural resolution continuing to occur up to one-year post partum.
If DRAM is normal why should I care about it?
The importance of this condition is widely debated among the literature. Currently there are many theories relating to the association of DRAM and physical impairment. It is important to note that none of these associations are proven in the literature and some of these theories actually have evidence to support no association! It is important to understand that DRAM during pregnancy is normal and for the majority of women will naturally resolve.
What theories does the evidence support?
There is a small amount of evidence to support the association of DRAM and negative body image and potential functional impairment of the abdominal wall. However even this evidence has limitations. An individualised approach is needed, as certain exercises may be appropriate for some, but not for others. Similarly, abdominal bracing/binding may be appropriate in some cases, but not in others.
How can I fix DRAM?
Current evidence suggests that to improve abdominal muscle function and appearance we may not need to decrease the gap as we once thought! Now, physiotherapy focuses on optimizing posture, improving muscle activation and function by empowering women through exercise!
For more information about exercise during pregnancy and postpartum recovery, book an appointment at Ahead Physiotherapy.
References:
(Dufour, Bernard, Murray-Davis, & Graham, 2019)
(Benjamin, Frawley, Shields, van de Water, & Taylor, 2019; Bø, Hilde, Tennfjord, Sperstad, & Engh, 2017; Lee & Hodges, 2016)
Benjamin, D. R., Frawley, H. C., Shields, N., van de Water, A. T. M., & Taylor, N. F. (2019). Relationship between diastasis of the rectus abdominis muscle (DRAM) and musculoskeletal dysfunctions, pain and quality of life: a systematic review. Physiotherapy, 105(1), 24-34. doi:10.1016/j.physio.2018.07.002
Bø, K., Hilde, G., Tennfjord, M. K., Sperstad, J. B., & Engh, M. E. (2017). Pelvic floor muscle function, pelvic floor dysfunction and diastasis recti abdominis: Prospective cohort study. Neurourology and Urodynamics, 36(3), 716-721. doi:10.1002/nau.23005
Dufour, S., Bernard, S., Murray-Davis, B., & Graham, N. (2019). Establishing Expert-Based Recommendations for the Conservative Management of Pregnancy-Related Diastasis Rectus Abdominis: A Delphi Consensus Study. Journal of Women’s Health Physical Therapy, 43(2), 73-81. doi:10.1097/jwh.0000000000000130
Lee, D., & Hodges, P. W. (2016). Behavior of the Linea Alba During a Curl-up Task in Diastasis Rectus Abdominis: An Observational Study. The Journal of orthopaedic and sports physical therapy, 46(7), 580-589. doi:10.2519/jospt.2016.6536
